Monkeypox has been declared a global health emergency by the World Health Organization and a public health emergency by the U.S. government. Increased access and support for testing, treatment, and vaccine supplies and other resources will be prioritized by the federal government and state and local health departments.
“While it’s possible for any individual to be infected by monkeypox, the risk is still very low given how it currently spreads,” says Eddie Stenehjem, MD, Intermountain’s senior medical director of Medical Specialties and infectious diseases expert. “Individuals and healthcare professionals shouldn’t panic and should take precautions, understand resources available, and follow guidelines for testing and treatment.”
Intermountain’s Infectious Diseases team has been staying on top of the situation and continues working with state health departments and local agencies to access available resources and support best practices. Ensuring physicians, APPs, and caregivers have clear and updated guidance is a top priority to preventing infection and delivering patient care. This article shares current guidelines for Utah. Information specific to other states and regions will be communicated to caregivers soon.
Review the latest information on monkeypox (or access the full Monkeypox Clinical Guideline):
- What is monkeypox?The monkeypox (MPX) virus belongs to the Orthopoxvirus genus that includes variola virus, which causes smallpox, the vaccinia virus, which is used in the smallpox vaccine, and the cowpox virus.
- Where are the outbreaks?The Centers for Disease Control and Prevention (CDC) is tracking an outbreak of monkeypox across several countries that don’t usually see the virus, including the U.S. Access the CDC’s situation summary, map, and case count information.
- How is monkeypox transmitted?Monkeypox is transmitted through close physical contact, including but not limited to sexual contact. Individuals, regardless of their sexual orientation, with more close physical contacts, including sexual partners, are at higher risk of exposure based on how it currently transmits. Monkeypox may also be transmitted through proximity to respiratory droplets and contact with contaminated clothing or bedding.
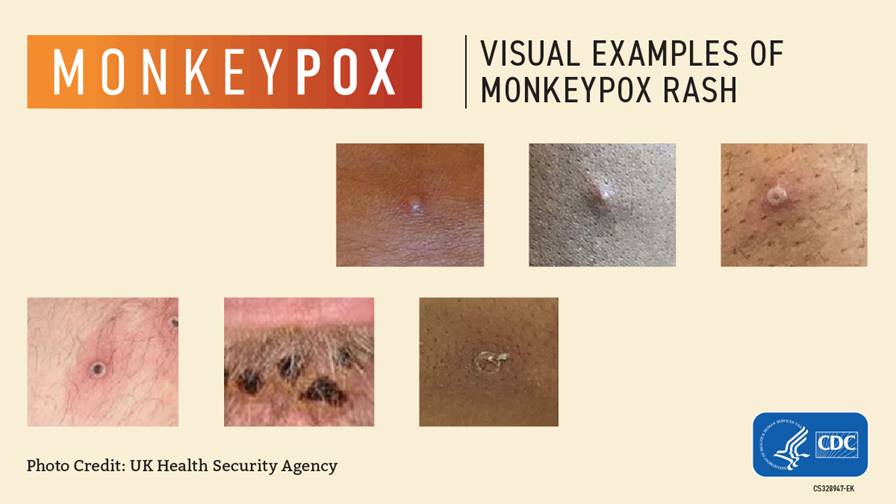
- What are the symptoms of monkeypox?Rash orskin lesions starting in genital or perianal areas that are similar in appearance to sexually-transmitted infections such as herpes or syphilis that can spread to other areas like the hands, feet, chest, face, or mouth. Other symptoms include fever, headache, muscle aches, exhaustion, and swollen lymph nodes.
- How can a physician or APP order a monkeypox test?Testing is critical to prevent transmission and provide timely therapy. Follow the Monkeypox Clinical Guidelines for ordering tests for patients with suspected monkeypox. Some highlights from the guidance:
- Tests should be performed through ARUP Laboratories predominantly, and ARUP will bill the patient and/or the patient’s insurance company for testing services. Only send clinical specimens for monkeypox testing to the Utah Public Health Laboratory if patients don’t have insurance or if there are significant financial considerations.
- To collect specimens, use contact and droplet precautions and wear proper PPE including surgical mask, gloves, gown, and good ventilation to protect yourself from infection. If a patient is hospitalized with suspected or confirmed monkeypox, admit the patient to an Intermountain facility with a negative pressure room and advance masking in an N95 or PAPR, in addition to wearing gloves and gown.
- What other testing might be appropriate? Genital, oral, and anal lesions of monkeypox can be similar in appearance to syphilis and the clustered lesions of herpes simplex virus (HSV) or varicella zoster virus (VZV). While the lesions of herpes simplex are generally more superficial and smaller, they may raise concern of monkeypox. Also consider sending syphilis serology, HIV testing, and separate swabs of the lesions for HSV/VZV PCR to your clinical laboratory. Don’t request a herpes or a VZV culture.
- How can monkeypox be treated? Tecovirimat (TPOXX) is an antiviral medication that was developed and ultimately FDA-approved for treatment of smallpox but is also likely effective against monkeypox. It works by blocking the virus from spreading from one infected cell to another. The CDC is making tecovirimat available through an expanded access investigational new drug (EA-IND) program for treatment of patients with, or at high risk of, severeor complicated monkeypox. For detailed drug information, the prescribing process, dosing, and safety, please refer to the TPOXX Prescriber Guideline document.
- Should I be vaccinated or vaccinate my patient?The CDC recommends two indications for monkeypox vaccination that are subject to specific instructions and target populations determined by local health departments: Pre-Exposure Prophylaxis (PrEP) or vaccination in high-risk groups to prevent disease—and Post-exposure Prophylaxis (PEP) or vaccination after exposure to monkeypox to prevent infection, when given within four days after exposure, or to limit severity, between four to 14 days after exposure but prior to infection. Jynneos, a live, replication-incompetent vaccinia virus vaccine that’s safe to give in HIV and other immunocompromised hosts, has been FDA-approved for monkeypox. Currently, Jynneos is being distributed to state health departments for use and is in limited supply. The Utah Department of Health & Human Services is working with local health departments (see department list and contact information) to match available supply to highest-risk groups. Currently, vaccine is being prioritized to individuals who have recently been exposed to a confirmed or suspected case, and men who have multiple male sexual partners.
Questions? For general questions or escalation items, contact your associate medical director, senior medical director, or other leader. Leaders should please contact the following: for testing questions, Bert Lopansri, MD, associate medical director of Infectious Diseases and medical director of the Microbiology Laboratory; for therapeutics questions, Brandon Webb, MD, Whitney Buckel, PharmD, or TPOXX@imail.org; and other questions, Eddie Stenehjem, MD, senior medical director for Medical Specialties.

