Use Intermountain Connect Care®
Learn More.
How can we help?
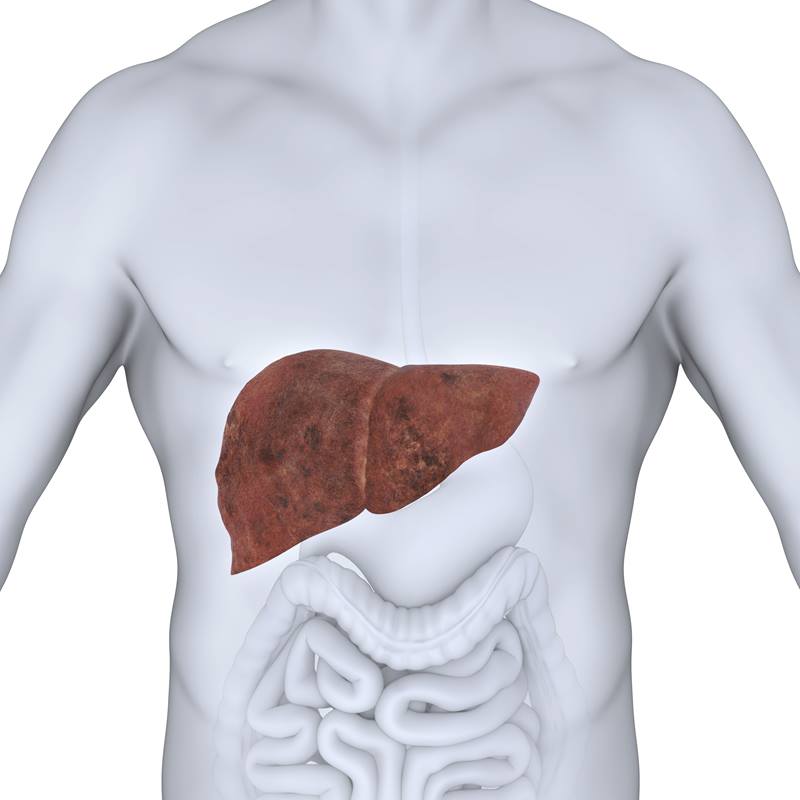
The prevalence of nonalcoholic fatty liver disease mirrors the rising trend of obesity in the United States. Globally, one in four people are living with the disease, which results when there is buildup of extra fat in liver cells that is not caused by alcohol. Nonalcoholic fatty liver disease is now the most common form of chronic liver disease.
For comparison purposes, stroke costs the United States about $34 million annually, roughly the same amount as NAFLD, according to the Centers for Disease Control and Prevention.
Identifying the economic burden of nonalcoholic fatty liver disease brings attention to the real need for readily-available treatments that will save money and lives, according to researchers.
For the study, researchers at Intermountain Medical Center in Salt Lake City examined medical records during a 10-year period (2005-2015) and identified 4,569 patients diagnosed with nonalcoholic fatty liver disease. A control group of 12,486 patients with no diagnosis of the disease was identified for comparison purposes.
Using integrated data from SelectHealth, the health insurance arm of Intermountain Healthcare, researchers analyzed the healthcare costs per patient and overall costs per year in both groups. The costs were then extrapolated to a national scale, which indicated an economic burden of $32 billion annually for the U.S.
Costs of the disease include:
• Inpatient hospitalization and outpatient appointments
• Emergency room visits
• Organ transplantation
• Mortality
• Medical procedures or new diagnoses
• New medications or changes to existing medications
“Our research is the first real-world estimate on actual healthcare utilization associated with nonalcoholic fatty liver disease in the United States,” said Richard Gilroy, MD, medical director of the hepatology and liver transplant program at Intermountain Medical Center. “The results highlight the major problem we face today and the potential tsunami we will encounter if we choose to not address the causes of NAFLD now.”
Nonalcoholic fatty liver disease occurs when fat is stored in liver cells. As the amount of fat in the liver increases, the disease progresses to nonalcoholic steatohepatitis, and is marked by liver inflammation and scarring that may cause irreversible damage. Left unaddressed, it can lead to liver failure. People who are overweight, have diabetes or who have a family member with liver disease should consider getting screened for nonalcoholic fatty liver disease.
“We are already in an era of escalating healthcare costs and we see what was an unrecognized and infrequent disease in the 1980s, is now a major epidemic that will further drive costs in years to come,” said Dr. Gilroy.
“Looking at the financial implications specifically, the results of the study also highlight the potential reduction in healthcare costs if treatments do become available,” added Michael Charlton, MD, with the Intermountain Medical Center transplant program and author of the new research study. “We currently have validated a predictive risk score that uses basic lab values and a patient’s medical history to allow us to predict which patients are at a higher risk of developing liver damage due to the disease.”
Researchers plan to use the prediction tool to get upstream of the problem at a population level by intervening with nutritional and therapeutic options, which may include clinical trials, before the patient reaches end-stage liver disease.
“At Intermountain Healthcare, we are looking to community initiatives to approach the issue as we know that change will only come through collaborations,” said Dr. Gilroy. “We believe that through our strong community relationships and initiatives, we will overcome this problem.”
Members of the Intermountain Healthcare research team involved in the study include Michael Charlton, MD; Li Dong; John Holmen; Richard Gilroy, MD; and Jake Krong.