What is an Ostomy?
If your intestine has had a disease or an injury, it may need
time to rest and heal, or it may need to be removed. If this
happens, you may be given an ostomy. An ostomy allows waste
to safely leave your body without passing all the way through
your intestines.
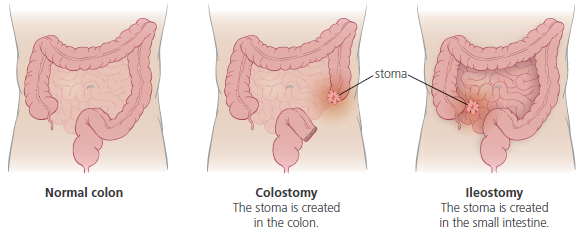
To create an ostomy, part or all of your colon is removed. A surgeon
brings a piece of your intestine through a small opening in your
abdomen. This opening is called a stoma. A stoma in the colon is a
colostomy. A stoma in the small intestine is an ileostomy. Body waste
passes through the stoma instead of the rectum. A disposable pouch is
placed over the stoma to collect the body waste.
Thousands of people of all ages, ethnic groups, and walks of life have
ostomies. For many people, the process has saved their lives. Most go
on to be healthy and productive.
If you have a colostomy, most of your intestine is still there. You will
absorb about the same amount of nutrients, and your stool will be thick.
If you have an ileostomy, you no longer have a colon. You will absorb
nutrients, but will need to replace electrolytes with what you eat and
drink. Ileostomy stool is often mushy.
Ostomy terms to know
- Colostomy: A surgically created opening of
the large bowel, which forms a stoma and
diverts body wastes.
- Enterostomy: Surgical formation of an
opening into the digestive tract.
- Ileostomy: A surgically created opening of
the small bowel, which forms a stoma and
diverts body wastes.
- Ostomy: A surgically created opening which
is made through the abdominal wall to divert
body wastes.
- Peristalsis: The normal motion of the bowel
that moves bowel contents through the bowel.
- Peristomal skin: The skin around the stoma.
- Stoma: The visible portion of the intestine
that is surgically brought out to the skin
through the opening in the abdominal
wall during your ostomy surgery.
Understanding Your Stoma
The stoma is the part of the intestine that you see on your abdomen.
The surgeon forms the stoma by rolling the end of the intestine back
on itself, like the cuff of a sleeve. The edges of the stoma are sewn to
the skin to hold it in place. Body wastes then pass to the outside of the
body through this opening.
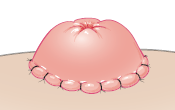
Here are a few characteristics of your stoma:
- It's red.
- It may bleed a little.
- It's always moist.
- Sometimes it moves.
- Its shape changes over time.
- It has no feeling.
- You can't control it.
Caring For Your Ostomy
At first, caring for your ostomy may seem like a lot of work.
With practice, though, it will become a natural part of
your day.
Getting help
You have a lot to learn at first. To get started, you may need help with:
- What products work best for you. There are many sizes and
options to choose from, and it will take a few tries to decide what
you prefer.
- Where to buy your supplies. You need to make sure your supply
company is covered by your insurance or Medicare plan.
- How to care for your ostomy. This booklet covers some
basic ideas. You’ll probably have plenty of other questions as you
get started.
Luckily, there are many places to go for help, so don’t try to do this
alone! Here are some places to get help:
- Your ostomy nurse at the hospital will get you started. Your nurse will help you 1) find what products work best for you, 2) buy supplies, and 3) care for your ostomy. Be sure to stay in touch with this or another nurse to help you along the way.
- Support groups. There are many people around you who
have gone through this already. The resources section on the
last page of this booklet lists support groups and web sites.
- Your supply company. They may have an ostomy nurse on staff.
Be sure to ask.
- Other materials. If you were given a video or other training
materials by your nurse, be sure to use them. These can be
very helpful.
Pouches and Barriers
The pouch and barrier are the two basic supplies for caring for your ostomy. Together they prevent odor
and protect the skin around your stoma. There are a few different types for you to choose from.
The pouch holds waste.
- A drainable pouch has
an opening at the bottom.
This type of pouch is used
most often with stomas
that have mushy or liquid
output. It can be emptied
and reused for three to five days.
- A closed pouch does not
open at the bottom. This
type is used with stomas
that output stool, which can
be difficult to squeeze out
of a drainable pouch. It is
thrown away after each use.
The skin barrier seals the pouch
to the skin around the stoma.
- On a one-piece system, the barrier
is already attached to the pouch.
You seal them to your skin at the
same time.
- On a two-piece system, you put
the barrier on your skin first, then
attach the bag in place over it.
Both one-piece and
two-piece systems can
be used with either
drainable or closed
pouches.
Skin Protection
The skin around a stoma is called peristomal skin. It should look
much like any other skin. Sometimes, however, this skin can become
red and raw. It’s easier to prevent skin problems than to treat them after
they happen. To keep your peristomal skin healthy, follow these steps:
- Change the barrier properly.
- Keep your skin clean.
- Use skin protection products if nececssary.
- Make sure the hole in the barrier is cut or molded to the right size.
Irritated Skin Care
Your peristomal skin may become irritated by one
of the following:
- Contact with stool or adhesives, or an allergic reaction to one of your
ostomy products.
- A barrier and pouch that have been left in place too long.
- A barrier that has been removed too forcefully and irritated the skin
or the hair follicles.
- Skin that has been scrubbed too hard.
- A fungus or yeast rash caused by persistent skin moisture or
from antibiotics.
If your peristomal skin becomes irritated, treat it right away.
To treat the irritation, create a crust that will make a barrier to absorb
fluid from the irritated skin and still allow your barrier to stick.
Here’s how:
- Wash the skin and pat it dry.
- Sprinkle stoma powder on the irritated skin. Brush off excess
powder to leave a light dusting. (Depending on the type of skin
problem you have, your nurse may recommend a different type of
powder to use.)
- Optional: Dab or pat the powdered skin with a skin-barrier wipe or
water. To avoid burning, use a no-sting skin preparation product or
one that is alcohol-free. Or, you can just use stoma powder alone.
- Repeat, if instructed to by your ostomy nurse.
- Allow it to dry, and then apply the barrier
If your skin is irritated and you have created a crust to help it heal,
you may have to change the pouch and barrier more often. Moisture,
powder, and skin preparations from a deeper wound often keep the
barrier from sticking.
If your skin continues to break down, becomes extremely irritated, and
gets sores, see your doctor or ostomy nurse.
Eating to Stay Healthy
For the first six to eight weeks after your surgery, you’ll need to eat
less fiber. Later, you can eat most everything you used to.
During the first six to eight weeks, both your intestines and your stoma may
be swollen. High-fiber foods may clump together and cause blockages
in the small intestine that will not easily pass through the stoma.
Blockages can be dangerous.
Eventually, you’ll probably be able to return to a normal diet that
includes the vitamins and nutrients you need to stay healthy. At first,
though, follow the tips below and in this table.
- Chew foods well. This will help you digest foods more easily.
- Be sure to drink something with every meal. This helps food pass
through the intestine more easily.
- Drink at least eight to ten glasses of fluids a day.
- Eat four to six smaller meals per day.
- Eat small servings. Eat your largest meal at noon and a smaller meal
in the evening. This will help reduce your stool output at night.
- After six to eight weeks, gradually increase the fiber in your diet until you
reach the amount needed for bowel control.
Eating to prevent food-related problems
Just as before your surgery, the foods you eat will affect the amount
of gas and odor you produce. They’ll also affect whether you have
constipation or diarrhea. With an ostomy, however, it’s especially
important to control these things. Learning the way different foods
affect you will help you have a better experience with your ostomy.
Constipation and Blockage
With an ostomy, you’re more likely to experience constipation,
blockage, or dehydration. Your body also absorbs medicine a
little differently than it used to. Understanding these issues can
help you prevent common problems.
Constipation
Constipation can affect anyone. Normally the colon absorbs water
into the body. When all or part of the colon is removed and an ostomy
is created, a lot of water passes out of your body before it is absorbed.
A person with an ileostomy can become dehydrated much more
easily. Dehydration can contribute to constipation in a person with
a colostomy.
Other factors also contribute to constipation. Stool consistency also
depends on what you eat, how often you eat, your emotions, and
sometimes medicines. Medicines that can cause constipation include
those taken for pain, to relax muscles, to calm nerves, and medicines
that contain iron.
Blockage
Blockage is a condition that affects people with an ileostomy.
A blockage happens when foods clump together in your small intestine
and clog it.
If you have an ileostomy, a blockage can become an emergency. A prolonged blockage could cause your intestine to rupture.
If the blockage lasts more than two or three hours, or if you start to
vomit, call your doctor right away, or go to the nearest hospital
emergency room.
Medications
Before you had an ostomy, medicine was absorbed into your
body through your intestines. Now it has less time in your
intestines to be absorbed. Anyone prescribing medicines for
you needs to do so with this in mind. They also need to
know what medicines you’re taking related to your ostomy.
- Remember to let your pharmacist, doctor, and dentist know
that you have an ostomy.
- If you have an ileostomy, do not take “long acting,”
“sustained release,” or “enteric-coated” medicines. Also avoid
medicines in hard-capsule form. If your doctor and your
pharmacist know you have an ileostomy, they can order
the kind of medicine that your intestine will handle best.
- If you have an ileostomy, don’t use laxatives. Your bowel
movements will already be soft and semi‑liquid. Make sure
your doctors know that you have an ileostomy so that they
won’t give you laxatives before a test or surgery.
- Some ostomy patients use bismuth preparations for odor
control. If you are scheduled for an x-ray of your bowel, you
must stop taking the bismuth for 24 to 48 hours before the
test. Bismuth shows up on x-rays and it may be necessary
to do the test over again if there is bismuth in your bowel.
- If you have questions or concerns about any medicine you
are taking, talk with your doctor or pharmacist.
Other Things to Consider
- Work. Ask your surgeon when it will be ok to return to work and other activities and about any special considerations you need to be aware of. Ask specifically about any concerns around contact sports such as football or soccer.
- Travel. Carry your supplies on in your carry-on bag when flying. The United Ostomy Association of America, Inc. (UOAA) has a downloadable TSA card to help alert the security team to your specific needs.
- Swimming. Swimming or even hot tub use is ok with an ostomy. For your protection as well as the protection of others, use a waterproof tape around the edges to help provide extra security and empty it prior to entering the water.
Support and Resources
© 2018 Intermountain Healthcare. All rights reserved. The content presented here is for your information only. It is not a substitute for professional medical advice, and it should not be used to diagnose or treat a health problem or disease. Please consult your healthcare provider if you have any questions or concerns.