As of October 3, Intermountain’s pulmonary and critical care team has identified 54 cases of vaping associated pulmonary injury.
Diagnostic criteria:
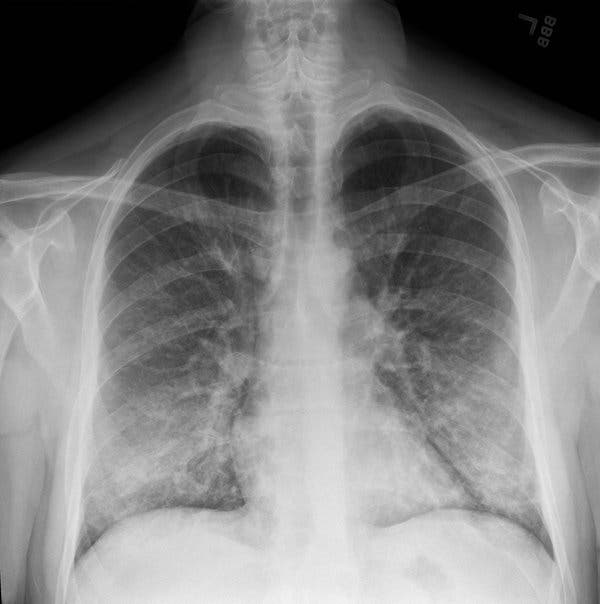
- Vaping within the past 90 days, bilateral infiltrates on x-rays, no infection and no other plausible diagnosis.
- Most patients have vaping within 1-2 weeks prior to presentation.
- Vaping - 90% THC oil, 10% nicotine and 50% both THC oil and nicotine.
- Detailed vaping history should be performed.
- Type of device(s) used (e.g. bottles, cartridges or pods)
- Specific type(s) of liquid used (e.g. nicotine, THC products, flavored fluids)
- Were devices, liquids, refill pods and/or cartridges shared with other people?
- Were old cartridges or pods reused with other homemade or commercial products?
- Were devices used to inhale drugs that were concentrated by heating prior to vaping (i.e., “dabbing”)?
- Details of vaping behavior (e.g. cloud volume, frequency of puffs, ‘zero’ or ‘stealth’ vaping, valsalva at end inhalation).
Epidemiology at Intermountain:
- 75% male, 90% are hospitalized, 20% are intubated, average age 28 (age range 18-54)
Presenting symptoms:
- Non-pulmonary symptoms include fevers, myalgias, nausea, vomiting, diarrhea, weight loss, back and neck pain. These symptoms typically have been present for 3-6 days prior to presentation and many times precede pulmonary symptoms. Initially patients are thought to have the “flu”.
- Pulmonary symptoms are cough, dyspnea, hemoptysis and tachypnea (rapid breathing). Some patients report very minimal pulmonary symptoms.
Evaluation:
- CXR (if negative consider chest CT scan) which show bilateral infiltrates c/w atypical pneumonia, viral pneumonia or pneumonitis. Chest CT scan typically shows ground glass opacities.
- Lab findings include negative serology for mycoplasma/chlamydia, negative urine legionella, negative sputum/blood cultures, negative respiratory panel (if severely sick/ICU), elevated WBC, mildly elevated LFTs, negative Procalcitonin (<2), elevated ESR and elevated CRP. If diagnosis in question, recommend pulmonary consultation.
Treatment:
- Antibiotics (Azithromycin 500mg daily for 3 days and Ceftriaxone for low DRIP score) for atypical pneumonia until bacterial infection is ruled out.
- When confident of diagnosis, system steroids are used. Dosing is dependent on severity of illness. Oxygen support with close monitoring.
- Vaping cessation counseling is imperative.
- Consultation with TeleCritical Care (801-442-8226) and/or pulmonary (if available at facility). The TeleCritical Care team serves as a resource and/or backup for clinicians seeing patients whom they suspect have vaping lung injury.
Follow-up:
After initial treatment, outpatient follow up is recommended in 2-4 weeks with CXR and DLCO.
Reporting Intermountain cases:
Intermountain cases are being tracked by Dixie Harris, MD – dixie.harris@imail.org; please send any new cases to her. She will report cases to the state. Remember to use PHI in subject line. Cases can also be reported directly to the state by contacting: Utah Department of Health at 801-538-9923 or CDCEISnml@utah.gov.
Useful resources:
- CDC: Severe Pulmonary Disease Associated with Using E-Cigarette Products
- CDC: Outbreak of Electronic-Cigarette–Associated Acute Lipoid Pneumonia — North Carolina, July–August 2019
- CDC: Outbreak of Lung Injury Associated with E-Cigarette Use, or Vaping
- NEJM: Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin — Preliminary Report
- ATS: Vaping: The Threat to Public Health and the ATS Response
- The American Academy of Pediatrics Issues Sweeping Recommendations on Tobacco and E-Cigarette

